A study carried out with a new human stem cell-derived model reveals that the most prevalent genetic risk factor of Alzheimer’s disease (AD), apolipoprotein E4 (APOE4), impairs the function of human brain immune cells, microglia. These findings pave the way for new, effective treatment approaches for AD. The results were published in Stem Cell Reports.
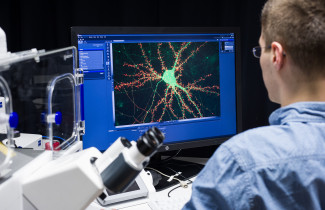
The study of human microglia has been hindered by the considerable challenges of isolating sufficient numbers of viable microglia from human brain tissue. The new study presents a protocol to differentiate patient-derived stem cells to produce large numbers of human microglia that closely resemble their in vivo counterparts and that can be studied under controlled laboratory conditions. The study was carried out at the University of Eastern Finland in collaboration with the University of Wollongong, Australia, and the University of Helsinki.
Alzheimer's disease, the most common cause of dementia among the elderly, is thought to be caused by the abnormal build-up of amyloid protein in the brain. However, it is not known exactly what causes this process. Amyloid build-up is characterized by accompanying damage to the neurons, leading to cell death and shrinking of the brain. There is no treatment to cure or slow down the progress of the disease. Several promising compounds in animal trials have proven to be disappointing in clinical studies with humans. Most efforts to find a cure have focused on inhibiting the production of amyloid proteins.
Microglia remove amyloid from the brain using a mechanism called phagocytosis, and they take care of other inflammatory processes in the brain. The growing body of evidence shows that there are important differences between humans and animals especially in inflammatory processes. In Alzheimer’s disease, the function of microglia is compromised, but it is incompletely understood why microglia are unable to remove toxic amyloid in patients. Instead, microglia either lose their normal function or activate adversely and increase the loss of neurons.
APOE4 is the strongest genetic risk factor for Alzheimer’s disease. Apolipoprotein, APOE, plays a critical role in the metabolism of lipids, such as cholesterol, and contributes to repairing neuronal damage in the brain. APOE is present in humans in three isoforms, and genetics determines which forms an individual carries. Only the APOE4 form predisposes for Alzheimer’s disease, and over half of patients carry this form. In humans, the APOE gene is abundantly expressed in microglia, but its role specifically in these cells is poorly understood.
In the present study, researchers showed that APOE4 increases the inflammatory response of human microglia, but at the same time reduces the ability of the cells to migrate and phagocytose pathogenic material. These functions are important for maintaining the brain homeostasis, to protect from pathogens and control the normal cell death that comes with aging. Moreover, the researchers were able to identify for the first time that APOE4 impairs the metabolic activity of human microglia. Together, these findings demonstrate that APOE4 has a profound impact on the basic functions of human microglia. The metabolism of microglia may open up new avenues for targeted treatment and prevention of Alzheimer’s disease.
The present study reveals a new, interesting observation for treatment: microglia may have a significant role in the progression of Alzheimer’s disease, independent from their ability to remove toxic amyloid build-up. Patient stem cell-derived microglia offer an exciting new tool enabling studies of molecular mechanisms in other brain diseases, too, as well as controlled studies of new targeted therapies.
For further information, please contact:
Early stage researcher Henna Konttinen, University of Eastern Finland, A.I. Virtanen Institute, [email protected]
Professor Tarja Malm, University of Eastern Finland, A.I. Virtanen Institute, tel. +358 40 3552209, [email protected]
Original article:
PSEN1ΔE9, APPswe and APOE4 confer disparate phenotypes in human iPSC-derived microglia. Stem Cell Reports (2019). Henna Konttinen, Mauricio e Castro Cabral-da-Silva, Sohvi Ohtonen, Sara Wojciechowski, Anastasia Shakirzyanova, Simone Caligola, Rosalba Giugno, Yevheniia Ishchenko, Damián Hernández, Mohammad Feroze Fazaludeen, Shaila Eamen, Mireia Gómez Budia, Ilkka Fagerlund, Flavia Scoyni, Paula Korhonen, Nadine Huber, Annakaisa Haapasalo, Alex W. Hewitt, James Vickers, Grady C. Smith, Minna Oksanen, Caroline Graff, Katja M. Kanninen, Sarka Lehtonen, Nicholas Propson, Michael P. Schwartz, Alice Pébay, Jari Koistinaho, Lezanne Ooi, Tarja Malm.
Published online 12 September 2019: https://www.cell.com/stem-cell-reports/fulltext/S2213-6711(19)30298-X