Digital pathology can increase equity in cancer diagnostics even globally, said Professor Anil Parwani at a Finnish Cancer Institute (FCI) Symposium in Kuopio.
Organised by the FCI, the multidisciplinary Cancer Research Community (Cancer RC) of the University of Eastern Finland, FICAN East and the Wellbeing Services County of North Savo on 26-27 September, the 16th FCI Symposium brought together world-renowned clinical experts and dedicated researchers to discuss the latest advances in the fight against cancer.
One of the topics was the use of digital pathology and AI, which, according to Professor Anil Parwani from Ohio State University, can make cancer diagnostics more objective and accurate.
Hospitals are increasingly adopting digital pathology, which means that instead of examining patient specimens on traditional glass slides under a microscope, pathologists more often use digital technology. Glass slides are scanned and converted into digital images that can be viewed and analysed on a computer. This has also opened up possibilities for computer assisted diagnostics.
“Digital images can be shared easily, so for instance, when a patient has a rare tumour, consultations can be made between experts even across the globe. Machine learning algorithms can decipher more information from digital slides than the human eye, providing additional clues as to which treatment may work for the patient. This to me is the next frontier of medicine,” Parwani said.
When a patient has a rare tumour, consultations can be made between experts even across the globe.
Anil Parwani

Even chemical staining of tissue samples, which is widely applied in cancer diagnostics, could be replaced by virtual staining. “It would reduce the use of chemicals, enabling more sustainable sample processing,” said Associate Professor Pekka Ruusuvuori from the University of Turku, who has developed the method in collaboration with Research Director Leena Latonen from the University of Eastern Finland.
Another advantage of virtual staining is that the sample can still be used for other experiments, which is usually not possible after chemical staining.
Digital pathology is just one area where AI-based methods can make a difference. “Cancer research is very data driven these days, and plenty of data are produced from multiple other patient measurements, down to molecular and genome level. Computational tools are crucial for interpreting all these data. However, we are still in the early days of actually bringing AI into actual patient level use, and such tools need to be carefully validated,” Ruusuvuori said.
“As there is a shortage of pathologists around the word, I’m afraid there may be a pressure to use AI tools as a solution to this problem. However, AI tools can’t replace pathologists and their use should be carefully regulated,” Parwani added.
New approach to predict immunotherapy response
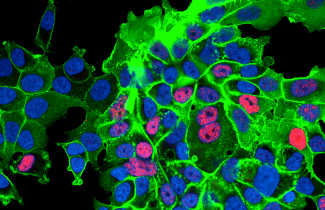
“Multiplexed imaging has allowed us to better identify, for instance, different immune cell types and their location in a tumour sample. With our new protocol, we can also see which cells communicate with each other,” said Charlotte Stadler from KTH Royal Institute of Technology, co-director of the Spatial Biology Platform at SciLifeLab in Sweden.
Her team uses multiplexed imaging based on fluorescent-dyed antibodies that attach to specific proteins in cells. “We have now integrated it with new technology enabling us not only to see which cells are close to each other but also if they talk to each other.”
“Specifically, we have been able to look at PD1-PDL1 interactions between cancer cells and immune cells.”
The programmed cell death protein PD1 expressed by immune cells and its ligand PDL1 in cancer cells are crucial in regulating immune responses in cancer. High amounts of PDL1 in cancer cells can prevent immune cells from attacking the tumour, so immunotherapy can be used to block PDL1. However, only a minority of cancer patients benefit from immunotherapy, whereas side effects can be severe.
In the best case, many unnecessary treatments, costs and adverse side effects could be avoided.
Charlotte Stadler

“Our preliminary data from a few urothelial carcinoma patients indicate that those who had more PD1-PDL1 interactions between cancer cells and immune cells were the ones that responded better to immunotherapy.”
Stadler hopes that further research will confirm the usefulness of this approach in the choice of treatments. “In the best case, many unnecessary treatments, costs and adverse side effects could be avoided.”
“Treatment resistance in cancers is an important and timely topic addressed in many presentations,” said UEF Docent Sanna Pasonen-Seppänen, who chaired the session focusing on the challenges of cancer heterogeneity.
She pointed out that immunotherapies, particularly immune check point inhibitors (ICI) such as PDL1 inhibitors, have revolutionised the treatment of solid cancers during the past decade. “However, there are substantial differences in the response likelihood to ICI therapy between different cancers and patients. To improve the efficacy of therapy, it would be essential to find novel predictive biomarkers for therapy response. The technology presented by Stadler offers one promising approach."
UEF Professor Anna-Liisa Levonen-Harju spoke about the role of transcription factor NRF2 in lung cancer. Lung cancer is one of the most common and aggressive cancer types with a dismal five-year survival rate of approximately 15 per cent. The vast majority of these are non-small cell lung cancers (NSCLC) which are genetically and morphologically very diverse, and therefore novel insights into their biology are urgently needed.
NRF2 regulates pro-survival genes and has been shown to be commonly overactive in lung cancer, but there are no targeted therapies towards the factor. “Importantly, NRF2 overactivity has been associated with poor responses to immune checkpoint therapies, which have become a first-line therapy in NSCLC,” Levonen-Harju said.
According to Levonen-Harju, NRF2 activity status could be used as a biomarker of therapy response. Recent research has shed light on the role of NRF2 in cancer cell-microenvironment interactions, and novel approaches are emerging to pharmacologically target NRF2.

Health and economic benefits from clinical trials and biobank samples
The number of clinical trials is decreasing in Finland, which means we are missing out on substantial economic potential and health benefits. “Clinical trials are integral in advancing science and the care of patients,” said Tuomo Alanko, Chief Physician at Docrates Cancer Center and one of the speakers in the session focusing on the impact of clinical research.
For example, the value of the treatment patients receive in one clinical trial is on average 1.2 million euros and the societal value for Finnish healthcare 10 million euros, according to a report by the health economics company ESiOR and Pharma Industry Finland.
“In the Well-being Services County of North Savo, each euro invested in clinical trials returned four euros,” added Erkki Soini, CEO of ESiOR.
Docrates is a private hospital that also performs clinical trials sponsored by the pharmaceutical industry. Alanko said some cancer patients actively seek clinical trials even abroad. Access to new treatments is valued, but he pointed out that patients need to be aware of the risks as well. Especially before enrolling for trials outside Europe, it’s important to find out about trial-related insurance coverage and follow-up care, among other things.
How to increase clinical research and to get more clinical trials to Finland? The session’s panellists, chaired by UEF Professor Arto Mannermaa, were unanimous on the need to integrate research in medical training and routine clinical practice, to allocate resources to clinical research and trials at hospitals, and to set up centralised clinical trial services as contact points for companies.
“Real-world data in real time are needed to gain information on the efficacy and costs of cancer therapies in routine clinical practice,” added Satu Tiainen, Director of FICAN East.

Efforts should be made to increase the representation of the older population in clinical trials, noted Tiina Vesterinen, Managing Director of the Foundation for the Finnish Cancer Institute. “The number of cancer cases is increasing especially among older people. However, at present they are greatly underrepresented in clinical trials, and those who participate are considerably healthier than the average older patient, so the study results cannot be generalised to the older population seen in daily clinical practice.”
Johanna Mäkelä, Director of Research and Services at Finnish Biobanks (FINBB) pointed out that the data from biobank samples could be used in cancer prevention and individualised care, in addition to research. In a recent project, genomic data on breast and ovarian cancer risk were returned to biobank donors who could then take part in intensified screening, consultations, and possibly preventive surgery. “This resulted in noteworthy health gains and was feasible and cost-effective. The data were welcomed as 70% of these people had not previously known of their genetic risk.”
Timo Toikkanen, who spoke as a patient representative in the panel, said he would have liked to hear about clinical trial options during the course of his treatment. “It would also be valuable if my biobank sample could help in choosing the best treatments for me. All the data on my cancer are in the biobank.”